Takeaway
Most healthcare professionals maintain high standards, perfectionistic tendencies, and critical minds. This appears to be an advantage in a high stakes-high risk work environment. However, these habits of mind may backfire when held too tightly and lead to emotional exhaustion. Being mindful can offset this problem.

| April 19, 2018 | 3 min read
By Patricia Dobkin, PhD, McGill University Department of Medicine
Cringe-worthy
Most of us cringe when we hear the word “role play.” Next, we slink back into our chairs hoping not to be noticed.
One such occasion comes to mind. During a Mindful Clinical Practice workshop, a mix of healthcare professionals were learning about communication stances, based on family therapist Satir’s model.
Satir’s model
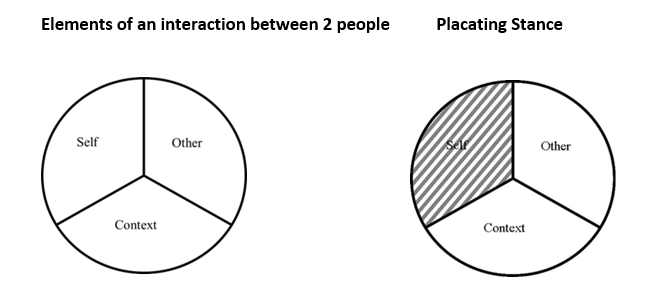
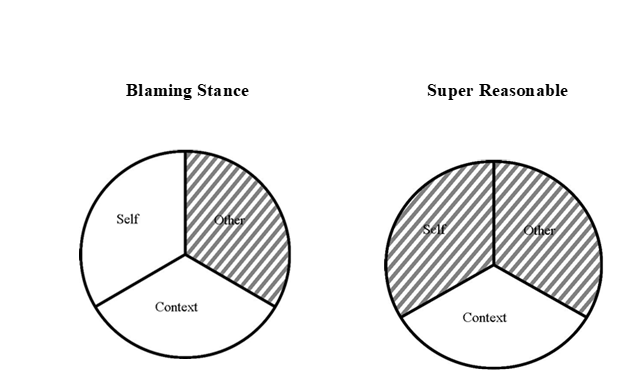
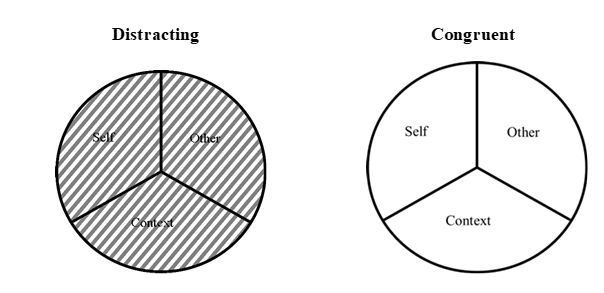
Satir identified three elements of any interaction between two people (self, other, context) and four common, often unconscious, stances that people tend to adopt that leave out elements of the interaction. The part that is left out is indicated by shading in the diagrams below.
The ideal way that’s recommended when relating to another person is congruence, where all elements are included.
The role play
I asked for participants to present a few examples of when they felt stuck in a clinical encounter and selected a scenario that would work well for teaching purposes.
The doctor who chose to work through a situation was a family physician. She included a nurse in the role play. Rather than play herself, she instructed another workshop participant to do so, enabling her to observe herself.
What surprised me was that she brought up a situation that had occurred early in her career. She had made a mistake on a medication order that could have killed the patient. The nurse had noticed it in time, but temporary damage had been done. Knowing that she had injected the medication and fearing for her job security, the nurse took a blaming stance (“You wrote the order!”) while the young doctor, ashamed about the error, thought to herself, “How could I be so stupid?!” apologizing profusely, taking a placating stance.
The scenario ran through the doctor’s mind, not only during that shift, but for years afterwards. The scene brought her to tears even though the patient survived.
If both had been more congruent, they could have talked about what brought about the error (e.g. all-night shift, both tired and less able to focus), how written records are more difficult to read then electronic ones, etc.
Debriefing the role play
What was most interesting was the debriefing that took place after the role play. The psychologists in the room were caring and supportive in a way that the doctor wasn’t used to. Unlike during some Morbidity and Mortality Rounds, the people in the room allowed space for her emotions. Tears weren’t viewed as a sign of weakness.
The doctor was touched by their concern for her well-being. They didn’t blame or shame her. Rather, they approached it as an example of vicarious trauma. They helped her to accept that it is human to err.
STOP and the Triangle of Awareness
Two teaching tools especially helpful for learning how to alter reactivity are STOP and the Triangle of Awareness, as they help the person choose a skilful way of dealing with a stressful situation or an interaction with another person.
STOP:
S = Slow down/Stop
T = Take a breath
O = Observe (use the Triangle of Awareness for awareness of the self, the other, and the context)
P = Proceed (respond rather than react)
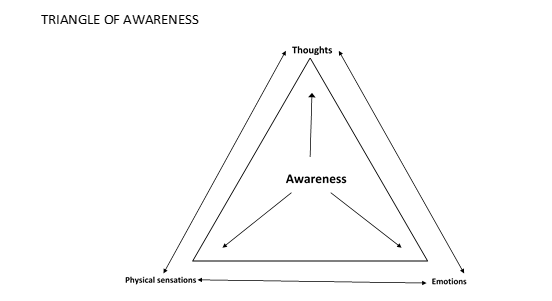
One becomes aware of how thoughts, emotions, and body sensations are connected; this insight allows one to change conditioned patterns.
For example, a clinician may notice his fatigue, how upset he feels about working overtime, and notices how he thinks the situation is unfair. Consequently, he may understand how this could impact his attitudes and behaviours when working with a patient in a busy outpatient clinic.
While teaching, the instructor models a nonjudgmental attitude and helps participants, who are often their own harsh critics, adopt a kinder attitude towards themselves and others.
Moving towards mindful congruence
Most doctors and healthcare professionals maintain high standards, perfectionistic tendencies, and critical minds. This appears to be an advantage in their high stakes-high risk work environment but, these habits of mind may backfire when held too tightly and lead to emotional exhaustion and beliefs that they are not performing well enough—two aspects of burnout. Being mindful can offset those problems.

